Depression is undoubtedly a major issue in New Zealand. Over half a million kiwis have been diagnosed with depression at one point in their lives, and one in nine adults are on prescribed anti-depressants. New Zealand also ranks NUMBER ONE in teen suicide rates amongst developed countries. How does this happen in this beautiful, free and peaceful country?
Causes of depression are complex and multifaceted. Numerous factors can contribute to the development of depression, such as bullying, traumatic experiences (both physical and mental), grief, illnesses, medications and other biochemical reasons.
For the last 60 years or so we had believed that the root cause of depression came from deficiencies in the neurotransmitters (signaling chemicals in our body responsible for mood and energy) such as serotonin, dopamine and noradrenalin, along with stressful life events. It was also commonly understood that neurotransmitter deficiency was a result of a defect in the genes coded for producing such neurotransmitters. This is called the monoamine hypothesis.
However, there are a number of research papers emerging recently that proves monoamine hypothesis to be inaccurate. A 2017 study from the Journal of Molecular Psychiatry concluded that there was no direct link between defective genes and the development of depression.
Perhaps this is why antidepressants don’t work sometimes. In fact, a survey conducted by Auckland University researchers with over 1800 participants noted that “Although 82 percent overall reported the drugs had helped, a 40 percent still felt either moderately to severely depressed”. A review of 70 studies in the British Medical Journal (2016) showed that a significant number of people had unwelcomed side-effects from taking antidepressants, such as sexual dysfunction, emotional numbness, feeling less positive, and it even doubled the risks of aggressive behaviour and suicide in under 18 year olds.
It is obvious, more than ever, that antidepressants are not addressing the root cause.
So what else could be causing depression?
As explained earlier, the cause of depression cannot be narrowed down to one single factor. It is multidimensional – an amalgam of psychological, physical and social problems that is a cocktail known as depression. In this article, I will be approaching this psychiatric disorder from another angle that you may have not thought of before… your GUT.
How could something, so far from the brain, be affecting my depression?
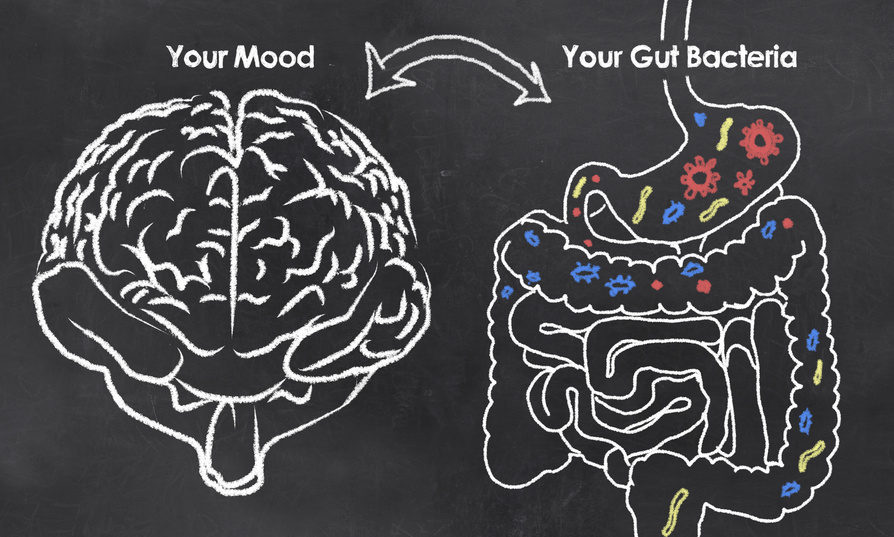
Your gut and your brain, in fact, is connected intimately through a two-way communication pathway called the Gut-Brain Axis. This pathway allows the brain to converse with the gut, and the gut to converse with the brain!
That’s right, your emotions, thoughts and feelings can affect your gut function.
Do you remember getting butterflies in your stomach right before an exam or speaking in front of a large crowd? You may also have experienced feeling rather “anxious” when you’ve had a stomach bug. These are only some examples of the gut-brain interaction. Irritable Bowel Syndrome is also worsened during the time of stress. Numerous studies have demonstrated the impact of psychological stress on gut sensitivity, movement and even permeability. Other studies have also shown that medications for psychological disorders can sometimes help to ease the IBS symptoms.
And what connects the brain and the gut so intimately is the bacteria we have in our gut.
There are over 100 trillion bacteria in our intestines, which makes up to roughly 1.4kg that we carry around with us every day!
These bacteria are paramount in the development of enteric (gut) and central nervous system in human beings, and plays a crucial role in sustaining a healthy communication between the gut and the brain. Your gut also produces up to 90% of the serotonin (the “feel good” neurotransmitter), along with other neurotransmitters that is found in the brain for regulating mood, memory, concentration, etc. This is why we call the gut your second brain!
And this healthy communication is maintained by a somewhat fragile balance between the good and the bad bacteria in the gut. Unfortunately, the lifestyle we lead today can disturb this balance. Stress, processed foods, medications, and toxic chemical exposures can all disrupt the gut, which ultimately affects our brain function.
For example, having loads of junk food, whilst having a stressful job, relationship issues and juggling part-time study, may cause high inflammation levels in your gut. The inflammation can then be carried into the brain. This inflammation can cause changes to your brain cells, such as the shrinkage of hippocampal neurons (brain cells responsible for mood and memory) and the growth of neurons in the amygdala (brain cells responsible for fear and survival instincts).
So how do we improve the gut, in order to improve depression?
Here are some simple tips to look after your gut health and improve the Gut-Brain Axis function.
Back to the basics
Many people are seeking answers as to “what” they should eat to keep their bowels happy. Whereas it is just as important as knowing “how” to eat your food. With our busy lifestyle, we barely have the time to chew, digest and enjoy our meals. If you want to improve your gut health, we must get back to the basics and learn how we used to eat!
- Do not drink water, or other beverages, during meals. This can dilute the acidity in the stomach required for adequate breakdown of food matters. Have your drink 30 mins before a meal (which can help stimulate your digestive enzymes and prepare the stomach for food) or 1 hour after the meal.
- Relax and take your time to eat your food. Especially for those who live a very busy lifestyle, it is important to shift your body from the “Fight/Flight” mode into the “Rest & Digest” mode during meals. Make sure to take adequate time for food, take your mind away from your busy lifestyle and enjoy your food.
- Chew your food. Chewing your food breaks down food material into smaller pieces, allowing your stomach and the rest of your digestive system to effectively digest and absorb your food.
- Aim to appreciate your food. Food is not just a fuel source for your body, but is there to be enjoyed. Notice the various combinations of taste, texture, smell and sight of your food. Building this habit will naturally encourage you to take your time and chew your food.
Avoid junk foods
Foods that are highly processed or high in sugar contents and trans-fats can alter your gut function for the worse. Processed foods such as packaged, ready-to-eat meals, takeaways and fast foods are often stripped of essential nutrients, and contain synthetic products such as artificial flavourings, colours, preservatives and flavor enhancers. Although it is tantalising to our taste buds, looks more attractive and lasts longer on the supermarket shelves, humans were not built to withstand the amount of unnatural, poor excuse for food we are consuming each day through the western diet. For example, some research shows that maltodextrin (a substance commonly used as a thickener) may trigger inflammatory bowel disease by making the bacteria stick more aggressively on the gut lining, and may also promote the growth of pathogenic bacteria such as Salmonella. High sugar foods such as fizzy drinks, fruit juice, snack bars, desserts, confectionaries and chocolate can feed and promote the growth of bad bacteria and yeasts in your gut (e.g. candida). Even coffee has adverse effects when you drink too much. It can reduce your ability to digest your food by hasting the emptying of your stomach and cause irritation along the intestinal tract due to its acidic compounds. Instead of eating out all the time, aim to cook mostly at home with fresh, preferably organic produce! Incorporate a variety of vegetables and fruit that provides good fiber content to assist healthy bowel movement and the growth of good bacteria in the gut. Avoid processed sugar most of the time and increase healthy protein sources (both animal and vegetable sources) and omega 3 fats, which will help to maintain the mucus lining of your gut.
Beware of medications
Certain medications are known to have side effects that may cause issues with the gut. In particular, oral antibiotics are the main culprits in disrupting the balance of your gut bacteria. Antibiotics are important, and have saved many lives throughout history. However, there is a global problem with over-prescribing in many circumstances, and patients are not well-educated on the appropriate gut care after antibiotic treatment. If you are having a course of antibiotics, make sure to take a high-quality probiotic supplement (20-25 billion, refrigerated) for at least 4 weeks, preferably for 3 months to restore the bacterial balance in your gut. Other medications, such as painkillers (paracetamol, codeine), oral contraceptives, antihistamines, heart medications, cholesterol medications and antacids can also cause gut issues if they are used long term. Consult with your doctor or a qualified health practitioner whether these medications are absolutely necessary, and how you can come off them safely. Please note that you should never stop medications without supervision of a qualified health practitioner.
Probiotics
There is a growing body of evidence that probiotic supplementation can significantly improve gut health, and in turn improve symptoms of depression. Probiotics containing specific strains such as Lactobacillus rhamnosus and Bifidobacterium have shown to reduce depression-related behaviours by affecting the neurotransmitters called GABA (an inhibitory neurotransmitter that helps to calm you down). A meta-analysis and systematic review (a study that reviews a large number of studies to draw conclusions) in 2016 also concluded that probiotics were associated with significant reduction of depression. Healthy bacterial balance in the gut can also be maintained by incorporating fermented foods in your diet. Foods such as sauerkraut, yoghurt, kefir, kombucha, kimchi, natto and miso are great sources of dietary probiotics. Although such foods do not contain enough probiotics to promote significant therapeutic effects, they are certainly great to maintain your gut health in order to reduce risks of developing depression.
If you are suffering from depression or know of someone who needs a hand, always seek help from a health professional first. The information provided here should be considered alongside proper support, such as counseling, medication or complementary services provided by a qualified practitioner.
If you would like to find out more about the connection between depression, inflammation, nutrition and the gut, please watch the FREE WEBINAR by clicking HERE
Kohei Iguchi
Qualified Naturopath, Medical Herbalist, Advanced Hemaview Practitioner.